In everyday life, we often do not appreciate the occasional aches and pains in the body. It was only when the pain developed to be excruciating and constant that we went to the doctor. This approach is fundamentally wrong, as it allows the disease to progress to severe. There are many pathologies of the skeletal system. One of them is shoulder osteoarthritis.
What is shoulder joint disease?
Osteoarthritis of the shoulder is a chronic disease related to cartilage degeneration.
The disease is easy to progress, causing dysfunction of the human musculoskeletal system. The influence of pathogenic factors leads to thinning of the cartilage, the appearance of cracks and its subsequent destruction.
Factors that lead to the appearance of shoulder joint disease
There are many factors that lead to the development of shoulder osteoarthritis. The main things are:
- vascular disease that leads to disruption of the proper blood supply to the joints,
- injury,
- heavy physical load on the shoulder joint,
- metabolic disease,
- genetic predisposition,
- diseases of the endocrine system,
- age-related changes in the joints,
- innate change
- extensive diseases of the musculoskeletal system,
- autoimmune diseases.
The risk group includes people over 55 years of age. This is due to age-related changes in the form of cartilage wear.
Progression of the disease
Depending on the gradual deterioration of a person's state of health relative to the course of the disease, signs of shoulder osteoarthritis of the 1st, 2nd, 3rd degree are distinguished.
First stage
The first stage is characterized by minor changes in the joints, pain when moving and lifting weights. This is due to a decrease in the elasticity of the cartilage tissue. The mobility of the joints is reduced, along with the patient's hand mobility is limited.
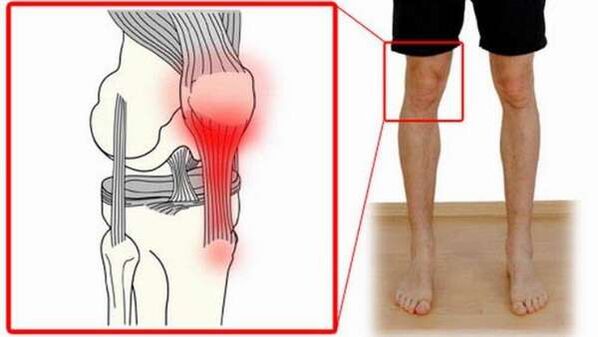
In the image, the doctor noticed that the joint space was slightly narrowed and the sockets appeared where the cartilage was thinning. With proper treatment, the first degree of osteoarthritis is terminated and the joint returns to a healthy state.
Second stage
If the patient does not pay attention to the symptoms of first-degree arthropathy, the second degree rapidly progresses, where it becomes difficult to restore the disturbed structure of the joint tissues.
The second degree has more pronounced signs. Joint space narrows to a minimum, clavicle and shoulder pain increases, becomes regular, crunches appear on hand movement, partial muscle atrophy, bone formation (osteogenesis) on filmX-ray.
The third stage
The final stage is manifested by changes in bone tissue, marked deformity, almost motionless joints, constant pain. If measures are not taken to prevent degenerative processes in the tissues, then there is a high probability of a complete violation of the motor activity of the hand.
Some patients have difficulty self-care. The level of the disease is considered the most difficult to cure requiring surgical intervention. The third stage of shoulder osteoarthritis is extremely rare. As a rule, it becomes the result of excessive total-body load on the damaged joint (for example, in professional sports).
Symptom
For a long time, hip-shoulder disease has no symptoms. In most cases, the first sign is acute pain. In the early stages of the disease, pain occurs rarely - from physical activity, from uncomfortable hand movements.
In the future, the pain increases, begins to appear at night with sudden movements, an uncomfortable position, then during the day, bothers more often and is systemic.
If treatment is not started in time, the feeling of stiffness when moving will be accompanied by pain. There is a click and crunch in the shoulder joints. This area is also often swollen, accompanied by an increase in the temperature of the whole body and in the area of the affected joints. Redness may appear on the skin.
Diagnose
If you experience neck and shoulder pain, contact your doctor who will conduct an initial examination and interview.
To diagnose shoulder osteoarthritis, people use the following methods:
- X-ray,
- Test,
- magnetic resonance imaging (MRI),
- computed tomography (CT) scan,
- ultrasound examination (ultrasound),
- scintigraphy - a method of functional imaging, which involves introducing radioactive isotopes into the body and obtaining images by determining the radiation emitted by them,
- arthroscopy - a method of imaging the joint cavity with a special optical device (arthroscopic),
- Thermometer is a method of recording infrared radiation of the human body.
Treatment
For many people who are facing this disease, the question often arises: is shoulder osteoarthritis curable forever? Treatment of any degenerative joint disease is aimed primarily at relieving symptoms and combating complications of the disease. It can only be completely cured by replacing the affected joint with an artificial joint.
Depending on the severity of the joint disease and the secondary causes that cause it, the treatment of shoulder arthropathy is indicated by a rheumatologist (in the early stages), an orthopedist or a doctor. orthopedic surgeon, surgeon, rheumatologist (with advanced forms of osteoarthritis). These are the main experts.
Auxiliary people include: therapist (general practitioner who performs treatment if not obtained from rheumatologist, orthopedist, surgeon), physiotherapist, physicianradiologist. Treatment for a patient will depend on the stage and cause of the disease.
Important! The disease belongs to the chronic number, so it is not necessary to say that the disease is completely cured. To date, there is no drug that can completely cure it.
Effective treatment includes the following methods.
Medicine
Treatment of shoulder osteoarthritis with drugs reduces the symptoms of the inflammatory process and relieves pain. For this, the following pharmacological groups are used:
- Non-steroidal anti-inflammatory drugs.
- Chondroprotectors.
- Analgesic.
- Glucocorticosteroid preparations. They are used as part of ointments and injections into the joints in the treatment of psoriatic arthritis of the shoulder.
In addition, antibiotics, complex vitamins and minerals, and other specific drugs used for treatment are prescribed by the attending physician, depending on the clinical picture of the patient's disease.
Physical therapy
Exercises aimed at strengthening the muscles of the shoulder are an indispensable element in the complex treatment of shoulder osteoarthritis. Exercises are performed at the end of the inflammatory process, in the period of remission.
Physical therapy helps restore joints, joint mobility, stop the progression of the disease, strengthen the affected apparatus and relieve pain.
Before starting gymnastics, prepare the muscles for the upcoming loads by warming up and stretching. A simple training complex includes the following exercises:
- In a sitting position, bring one hand behind your back, the other - from the side, stretch. Place your hands on your knees and relax. Do it slowly.
- Lift shoulders alternately and simultaneously. Do it 10 times.
- Movement of the shoulder forward and backward, alternately and simultaneously. Run 10 times.
- In a sitting position, hang your arms and relax. Do a swing back and forth without bending your elbows. Repeat 10 times with each hand.
Especially popular are the author's methods of treating joints. This exercise therapy is done in specialized centers, but is easy to do at home.
A feature of physical exercises is the focus on restoring the entire musculoskeletal system, not just the mobility of individual joints.
Physical therapy
Physiotherapy is included in the complex of measures for the treatment of deformed joints. It is effective in the early stages of the disease. Drugs and physical therapy for cervical spondylosis and shoulder osteoarthritis are prescribed by a doctor after examination and diagnosis.
Physical therapy treatment includes:
- ultraviolet irradiation,
- UHF therapy,
- acupuncture therapy,
- ultrasound therapy,
- amplipulse therapy,
- therapeutic baths,
- healing mud.
Surgery
When the on-going treatment measures do not bring positive motivation and the disease progresses, surgical intervention is indicated.
The following types of operations can be performed:
- Shoulder arthrocentesis is a minimally invasive procedure that allows the removal of inflammatory fluid from the joint cavity and the introduction of medication into it.
- Arthroscopy is performed using a video camera by perforating the joint area. This treatment option relieves symptoms without the long recovery period following surgery.
- Internal medicine - replacement of damaged areas of the joint with artificial elements.
Folk remedies
In the treatment of joint deformities, folk remedies are commonly and widely applied at home. However, keep in mind that alternative treatments should be used in addition to primary drug treatment.
The following herbal formulas are effective:
- Elecampane tincture for grinding. Stimulates blood circulation, relieves pain. To prepare it, 100 g of the dried root of the plant is mixed with 250 ml of vodka and applied to the affected area no more than five times a day.
- Compress oatmeal. Reduce pain syndrome. It is prepared as follows: a spoonful of oatmeal is poured into 500 ml of water, put on high heat and boil for about 10 minutes. The prepared mass is cooled to a temperature suitable for the skin and applied to the gauze. Such a swab is applied to the affected joint for one to two hours.
- Apply salt. Slows down the inflammatory process. Preparation: dissolve 50 g of salt in two cups of water. Dip a gauze pad in the prepared solution for three hours, then wring it out, heat it and apply it to the painful joint until the bandage cools completely.
Prevent
To prevent the onset and later progression of dry shoulder disease, it is important to follow simple rules for the prevention of the disease. Including:
- maintain an active lifestyle,
- take long walks regularly
- gymnastics, gymnastics, yoga,
- give up bad habits (smoking, alcohol),
- hot and cold shower,
- swimming,
- weight control,
- proper nutrition,
- prompt and thorough treatment,
- avoid injury, overexertion, hypothermia.
Conclusion
Shoulder degenerative deformity significantly reduces the quality of life of people, reduces mobility of the musculoskeletal system and causes discomfort with increasing pain. This disease cannot be completely cured, but the full use of treatment and prevention measures with a high probability of causing the disease not to go into remission.
The outcome of arising joint pathology depends entirely on the person, his or her willingness to regularly participate in therapeutic exercises and adhere to preventive measures. A person with this diagnosis can lead a full life.



























